Getting Tested for COVID-19: what happens at a coronavirus clinic
All the details
Getting Tested for COVID-19 is probably now the first thing you think about if you wake up with a sore throat or a fever. What does coronavirus feel like? With no experience of what the virus does to the body, and with symptoms that are similar to other illnesses, it’s impossible to know whether you have the coronavirus or not. One NSM was tested recently and shares her story.
Should I get tested for coronavirus? The symptoms that worried me
- Day One: On Saturday 14 March I started coming down with something; I could feel it in my sore throat, and I developed a tickly dry cough.
- Day Two: Sunday I was tired and coughing consistently, and so fatigued I slept from 11am-4pm with my phone going off right next to my ear while I slept through it. That night I was feverish and sweaty and slept badly, as the coughing became more pronounced.
- Day Three: By Monday the cough had taken hold and was making my chest rattle. I could hear wheezing and crackling my chest when I breathed. I slept most of the day again, and during the night I was woken by bouts of coughing every hour or so. I had a sweaty sleep in between, and then chills. I also developed joint pain.
- Day Four: Tuesday was test day. By now my cough was loud and hacking, my muscles ached from the cough, and I was dizzy and feverish. I had been taking Panadol for the discomfort. I was growing concerned that the length and severity of the symptoms might mean I had coronoavirus.
GETTING TESTED FOR COVID-19: INSIDE A CORONAVIRUS CLINIC
Getting tested for COVID-19: The First Steps
Because of my symptoms and because of multiple confirmed cases in my circle of contacts, I decided to investigate whether I could (or should) be tested.
First, I placed a call to the national 24-hour COVID-19 hotline on 1800 020 080. Expect to wait some time; I placed my call at 6.40am and it was 90 minutes before I had spoken to someone and gained their advice; this was also far earlier in the crisis when resources were less strained.
You may elect to visit your GP for assessment, but I preferred the hotline as:
- I felt terrible and unable to front up to a doctor’s office (a phone call from my bed was much easier)
- I was not sure GPs would be willing to see me if I was infectious, or if I should call ahead, or go to a different GP to my normal doctor
- I was worried about potentially passing the virus on if in fact I had COVID-19
- I knew getting tested for COVID-19 would not be done at a GP office, only at a purpose-built clinic
On the call, the crisis line worker asked me about my symptoms in detail, which were: a cough, fatigue, slight fever, joint and muscle pain.
She asked whether the cough had left me gasping for breath, whether I had trouble catching my breath and other specific questions to determine what to do.
Then, she checked if I met the criteria for testing:
- Had I been in direct contact with a confirmed case
- Had I returned from overseas in the last 14 days
Based on my symptoms, she recommended I attend an in-person walk-in coronavirus clinic immediately, and checked that I would be able to drive (so no risk of infecting others on public transport), would be wearing a mask (I had a P2 mask at home from the bushfire haze crisis). She reminded me not to touch anyone, or anything, to wash my hands frequently, and avoid touching my face.
Getting tested for COVID-19: Where are the clinics?
The crisis hotline worker listed various locations available at the time:
- Westmead Hospital
- Royal Prince Alfred (RPA)
- Canterbury Hospital
I attended RPA, specially set up for those getting tested for COVID-19. There are now many clinics closer to the North Shore, and you can see a full list here.
Please be aware there is a strict criteria for anyone getting tested for COVID-19. The reason given is to make sure tests are allocated as best they can be, and to manage staff and healthcare resources. Turning up to be tested when you don’t meet the criteria may mean you are turned away from a clinic, even if your GP has sent you to be checked. Please listen to your medical advisor and comply.
What happens when you go for testing?
Stage One: Arrival and register
At RPA, the clinic is at the back of the building behind the emergency department. Like any clinic, the area is cordoned off with tape and ropes, and at RPA two personnel are at the entry way dispensing hand santitizer and checking the participants are wearing masks, and at the clinic itself more workers in masks and gowns are stationed at the doors.
In the first waiting area, you are required to register, which means filling out your initial forms and hand them to the staff who are wearing protective gear.
The questions cover the same areas – personal details, symptoms, your usual doctor and whether you are in a high-risk category (eg returned traveller).
Hygiene is excellent. The chairs are over a metre apart and the staff wipe down everything you touch, including your seat after you go inside for stage two.

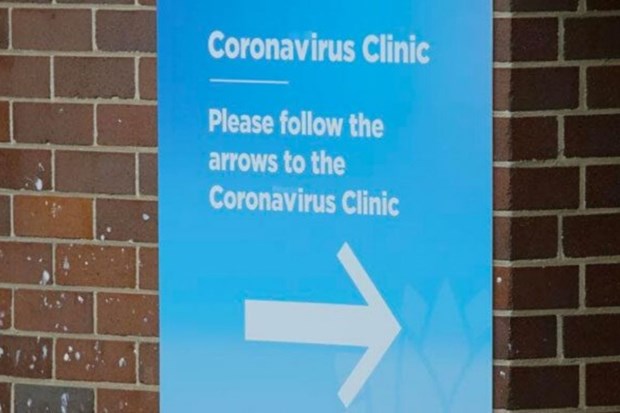
THE PATH TO THE COVID-19 CLINIC IS MARKED BY A BLUE LINE
THE FIRST WAITING AREA FOR REGISTRATION IS UNDERCOVER OUTDOORS

PATIENTS FILL OUT FORMS AND HAND THEM TO STAFF IN PROTECTIVE GEAR
Stage Two: Waiting chamber and eligibility test
Once past the sign-in, you move into an inside clinic waiting area. The room is divided into heath care workers and general public waiting for tests.

LOOKING INTO THE WAITING ROOM FROM OUTSIDE THE WINDOW

ONCE INSIDE, THE INSIDE ROOM HAS A LARGE WAITING AREA WITH WELL SPACED CHAIRS AND WAS CALM
Again, the spacing is deliberately wide and your area is sanitised after you vacate by efficient staff in protective suits.
I waited in this area for perhaps an hour, on a day with around fifty people presenting. While I waited a healthcare worker came and checked my details and confirmed I was in direct contact with a confirmed case, or that I had been overseas in the last two weeks.
Many people waiting were sent home without testing, because they did not meet the criteria. For example:
- An older man with a cold referred to the service by a GP but who had no contact with a confirmed case, or any overseas travel
- A young professional asked to come by an employer to be cleared for work
- A partner of a young woman undergoing testing; non-COVID-19 test cases are not allowed to wait in the area for obvious reasons
Target groups for testing:
- Recently returned travellers with symptoms
- Close contacts of confirmed cases
- Patients admitted to hospital with respiratory illness were target groups for testing
There has been ongoing tension over testing, with NSW Chief Health Officer Kerry Chant urging people without symptoms not to seek healthcare.
“If we’re swamped with testing that is low value, low yield, there could be delays finding those cases that are actually putting the community at risk,” she said.
Stage Three: The Tests
If you meet the criteria, after a short wait you are called to a sidechamber test area where your symptoms, details and testing criteria are checked again.
Two workers take your temperature under your arm, and then move you through to a smaller internal chamber with 13 seats marked out, and assign you one.

THE BOUNDARIES FOR SOCIAL DISTANCING ARE MARKED IN BLUE TAPE

THE SPACED AND NUMBERED (13) SEATS PREVENT CROSS INFECTION
You wait on your individual chair until you are called through to a one-person room with another worker in protective gear.
I had my nose swabbed (with a long, thin swab) – yes, both nostrils! And a mouth swab. The test takes about 20 seconds and then you’re free to go.
Getting tested for COVID-19: The results
I was advised a public health representative would contact me within 72 hours, but when nobody had called I ended up ringing myself on day 4.
I called the Coronavirus hotline, then a public health division before being referred to an assigned centre for my results.
The result? Negative, which came as a relief. I had been self-isolating since the prior Thursday but was still relieved my family and I were not positive.
Republished with permission from North Shore Mums.

Eliza Scanlan is a contributor with Practical Parenting. Eliza has written for several digital titles including New Idea Food and New Idea, with a passion for consumer and shopping news. Eliza is also a contributor for the Trolley Watch and The Flawsome Mum podcasts. In her spare time, Eliza loves watching Netflix and tending to her horses.